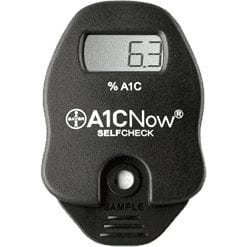
 Bayer A1C Now Self-Check System: If you have diabetes then you have to check your blood glucose quite regularly and there is no better way to check it accurately and regularly than to have an updated blood glucose monitor.
Bayer A1C Now Self-Check System: If you have diabetes then you have to check your blood glucose quite regularly and there is no better way to check it accurately and regularly than to have an updated blood glucose monitor.
There are a lot of issues with out-dated blood glucose monitors and one of those issues is irregular readings. If you monitor is old, it may give off readings that just don’t sound right and you may actually be making your diabetes much worse.
Another major concern to those using glucose monitors is the pain that they feel with each prick to measure their levels. It can actually be quite painful when you have to test 3-4 times a day.
The last issue that many people face when it comes to their monitor is the fact that it becomes more of a hassle to use than other glucose monitors today. You have change out lancets every time you test, you have to clean up the monitor itself, not to mention the fact that you have to place the testing strip into that tiny opening in the monitor. It all becomes a huge hassle that many people tire from quickly. You also must write down each and every reading and many people tend to forget that part.
With the Bayer A1C Now Self-Check System, all the problems are thrown to the wayside. You are getting one of the most highly advanced monitors on the market and what can be better than that?
First off, this monitor measures your A1C level which is very important when looking at diabetes. A1C measures your average blood glucose level over the past 2-3 months, which is said to be very important and is recommended by the ADA (American Diabetes Association) to be below 7 percent. However, this monitor is not for daily use, it is used to look at the big picture when it comes to measuring diabetes as a whole but is still very effective.
Here are some of its great features of the Bayer A1C Now Self-Check System:
- Easy to use
- Portable
- Needs only a small sample of blood
- Gets results in five minutes
- Can be used with a flexible spending account
- Gives on the spot feedback to patients
- Needs no maintenance
- Lab accurate
- National Glycohemglobin Standardization Program Certified
- Allows face to face communication with patients
- Bayer A1C Now Self-Check System kit includes: 1 A1C Now Self-Check Monitor, 2 single cartridges, 2 shaker kits, 1 quick reference guide, 1 overview and helpful hints booklet, 1 instructional DVD and 1 extra lancet.
The Bayer A1C Now Self-Check System is a great monitor that will monitor your A1C level and that’s important because with even as much as 1 percent reduction, many issues and complications that diabetic patients face can be lowered.
Measuring your blood sugar level as a diabetic is very important and many cannot always measures theirs as much as they would like but with more advanced products coming out all the times, everyone is sure to be able to get an accurate reading so that diabetic complications are no more of an issue.
 V-Go Disposable
V-Go Disposable  Accu-Chek Aviva Nano: Monitoring your blood sugar levels is very important and when a diabetic patient is unable to check their blood sugar, it can cause some other health issues such as retinopathy or
Accu-Chek Aviva Nano: Monitoring your blood sugar levels is very important and when a diabetic patient is unable to check their blood sugar, it can cause some other health issues such as retinopathy or 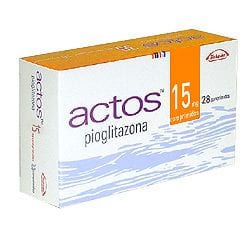
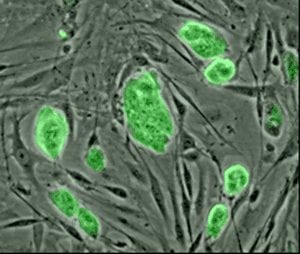 Diabetes Cure:
Diabetes Cure: 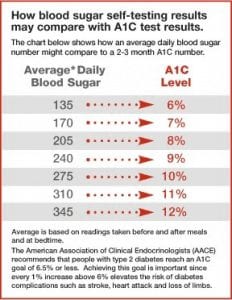 Is Tight Blood Sugar Controls Best for Type 2 Diabetes: Should persons with type 2 diabetes keep their blood sugar levels under strict control, resulting in their
Is Tight Blood Sugar Controls Best for Type 2 Diabetes: Should persons with type 2 diabetes keep their blood sugar levels under strict control, resulting in their  Diagnosing Diabetes and
Diagnosing Diabetes and  Nuts Over Carbs for Diabetes: A recent study shows that when those dealing with type 2 diabetes switched out some of their regular carbohydrates for a half cup of mixed nuts each day, the participants’ blood sugar levels and LDL cholesterol levels dipped slightly over three months. This is no reason to eat nuts all day long, but it’s a good enough reason to think about throwing in some nuts in place of the carbs each day.
Nuts Over Carbs for Diabetes: A recent study shows that when those dealing with type 2 diabetes switched out some of their regular carbohydrates for a half cup of mixed nuts each day, the participants’ blood sugar levels and LDL cholesterol levels dipped slightly over three months. This is no reason to eat nuts all day long, but it’s a good enough reason to think about throwing in some nuts in place of the carbs each day. New Study On Aspirin and Diabetes: A baby aspirin a day can help prevent a heart attack, according to the experts. If you are in the throes of a heart attack, it is recommended that you take a chewable aspirin. We all know there are numerous cases where the use of over-the-counter aspirin can be helpful to the extent that it can save lives.
New Study On Aspirin and Diabetes: A baby aspirin a day can help prevent a heart attack, according to the experts. If you are in the throes of a heart attack, it is recommended that you take a chewable aspirin. We all know there are numerous cases where the use of over-the-counter aspirin can be helpful to the extent that it can save lives. Linagliptin (Tradjenta) Possible Approval for Use in Europe for Type 2 Treatment: Linagliptin (sold under the name Tradjenta) has been available in the United States for those with type 2 diabetes since May 2011, when the Food and Drug Administration gave their approval for its use at that time. Tradjenta is an oral
Linagliptin (Tradjenta) Possible Approval for Use in Europe for Type 2 Treatment: Linagliptin (sold under the name Tradjenta) has been available in the United States for those with type 2 diabetes since May 2011, when the Food and Drug Administration gave their approval for its use at that time. Tradjenta is an oral