 Defining Neuropathy And How It Relates To Diabetes: Diabetics have to endure various medical conditions in conjunction with their diabetes. One such condition which may occur in diabetics is neuropathy, or nerve damage as it is more commonly known. In fact, approximately 50% of diabetics will experience some type of neuropathy. The following will discuss the condition of neuropathy and how it pertains to diabetics.
Defining Neuropathy And How It Relates To Diabetes: Diabetics have to endure various medical conditions in conjunction with their diabetes. One such condition which may occur in diabetics is neuropathy, or nerve damage as it is more commonly known. In fact, approximately 50% of diabetics will experience some type of neuropathy. The following will discuss the condition of neuropathy and how it pertains to diabetics.
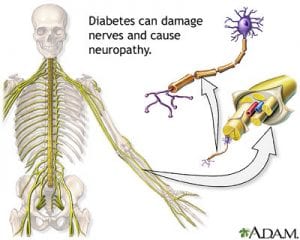
What Is Neuropathy
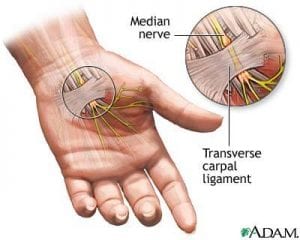
Neuropathy is damage which occurs to the various nerves within the body. When the nerve damage occurs as a result of the diabetes it is more specifically known as diabetic neuropathy. There are various types of neuropathy including sensorimotor neuropathy, autonomic neuropathy and focal neuropathy. Sensorimotor neuropathy is sometimes called peripheral neuropathy and can lead to tingling, pain, numbness and even weakness in the hands and feet. Autonomic neuropathy has symptoms which are a bit more serious and may consist of vomiting, bladder problems, diarrhea, digestive problems, elimination of low blood sugar warning signs, dizziness, sweat gland issues and changes in the eyes pertaining to reaction to light. As for the focal neuropathy, this type of nerve damage can lead to double vision, paralysis on the side of the face and pain throughout the body.
How Does Neuropathy Relate to Diabetes
Diabetic neuropathy is caused by the frequent high blood sugar levels in the body. Those who have more episodes of high blood glucose levels will often be more likely to experience diabetic neuropathy. How much nerve damage one sustains will depend on various factors such as length of time being diabetic, severity of the diabetes and how old you are. Alcohol is another factor relating to diabetics becoming susceptible to neuropathy as those who drink a lot will be more likely to sustain nerve damage than those who have an occasional drink or do not drink at all.
Diagnosis Of Diabetic Neuropathy
If you are diabetic and wondering if neuropathy is an issue for you, there are a few ways in which doctors diagnose diabetic neuropathy. Simple tests such as sensitivity to touch and temperature will be performed. More clinical tests including having an electromyogram and nerve conduction studies performed will pinpoint whether any types of nerve damage have occurred. By discussing your individual symptoms with your doctor, it will make it easier for the medical health professional to diagnose the type of nerve damage and the severity thereof.
Prevention Of Diabetic Neuropathy
The main way to prevent the occurrence of diabetic neuropathy is to keep your blood sugar level in check. Always be sure to monitor your blood glucose level and take the insulin as soon as it is needed. Maintaining a healthy diet and engaging in a reasonable amount of exercise will help to keep your blood glucose level steady. There are a wide array of diabetic cookbooks on the consumer market these days which can help with eating healthy and enjoying your meals at the same time. It is also imperative that diabetics keep a healthy and consistent weight as this too will help to keep blood glucose levels in target range.
Treatment Of Neuropathy Experienced By Diabetics
With regard to specific treatment methods, how the nerve damage is treated will depend on the symptoms which the diabetic is experiencing. For example, those who are experiencing pain may be given pain-relieving medications and those who have digestive problems may be prescribed medicines which treat such conditions. The treatment will be on a symptom-by-symptom basis as this is the best way to deal with any problems which may arise as a result of the neuropathy. As stated above, the doctor will recommend that the individual eat healthy, exercise and maintain a target weight to keep neuropathy and its accompanying symptoms at bay.
 The medical condition known as
The medical condition known as 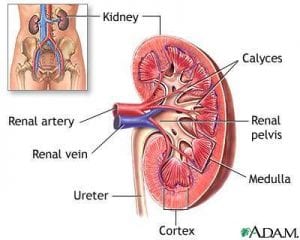 Treating
Treating 