 A small retrospective study recently presented at the annual meeting of the European Society for the Study of Diabetes has demonstrated that elevated accumulation of fat, inflammation, and fibrosis of the liver are associated with a higher risk of cardiovascular disease. The risks are especially high for those who have been diagnosed with diabetes.
A small retrospective study recently presented at the annual meeting of the European Society for the Study of Diabetes has demonstrated that elevated accumulation of fat, inflammation, and fibrosis of the liver are associated with a higher risk of cardiovascular disease. The risks are especially high for those who have been diagnosed with diabetes.
“What we are realizing is that [nonalcoholic fatty liver disease] is adding extra cardiovascular risk to people with diabetes, and to those without, on top of that which is already existing,” says Dr. Christopher Byrne, a lead investigator working on the study.
Dr. Byrne, who is a professor of endocrinology and metabolism at the University of Southampton in England, suggested that the findings of the study demonstrate that patients who have documented liver disease may require more aggressive therapies in response to the additional risk they face. Those therapies should target the liver in addition to the heart.
The study was conducted on 112 patients who had been diagnosed with nonalcoholic fatty liver disease, proven by biopsy. The study showed that the participants’ Kleiner scores were highly-correlated with Framingham Risk Score (FRS) as well as QRISK2 — both indicators of cardiovascular risk. The Kleiner score is a histologic measure of non-alcoholic fatty liver disease severity.
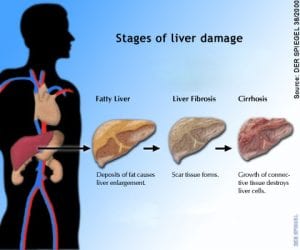
“Nonalcoholic fatty liver disease represents a spectrum of fat-mediated liver conditions causing progressive hepatocellular damage,” says Sarah Hudson, a medical student at the University of Southamptom. “There is increasing evidence of an increased cardiovascular risk associated with progression of nonalcoholic fatty liver disease,” continued Hudson. She also noted that the preferred method of determining the severity of non-alcoholic fatty liver disease was through histopathologic tests.
The primary goal of the study was to determine whether Kleiner score is correlated with risk of cardiovascular disease and whether the score was higher in individuals who were already known to have increased cardiovascular risk, especially those who had also been diagnosed with diabetes.
Kleiner scores provide an assessment of a variety of factors, including steatosis, lobular inflammation, fibrosis, and hepatocyte ballooning. As liver disease becomes more severe, Kleiner score increases correspondingly.
The mean age of participants in the study was 48 years; mean Kleiner score among the patients was 5.3, while median FRS and 13 and median QRISK2 score was 8. Mean body mass index (BMI) of the participants was about 34kg/m2.
Not only were Kleiner scores found to be highly-correlated with cardiovascular risk according to both FRS and QRISK2 models, but they were also higher in a group of 32 participants who had been diagnosed with diabetes versus non-diabetic individuals. It was discovered that the increased risk of cardiovascular disease in correlation with non-alcoholic fatty liver disease was independent of hyperglycemia and increased body weight.
“We need more prospective studies to see what markers may be used to help stratify who requires biopsy and how best to manage people who have got NAFLD,” noted the study’s authors.
“Up until now we’ve been very poor in providing cardiovascular risk reduction treatments for patients with NAFLD,” said Dr. Byrne. “But what we don’t know is whether those lifestyle changes are good at decreasing liver inflammation, or decreasing liver fibrosis.”
Dr. Byrne, along with other members of a research team, are now studying the use of highly-purified omega-3 fatty acid ethyl esters in the treatment of fatty liver disease. This form of fish oil has been available in Europe for at least a decade as Omacor and in the United States as since 2004 as Lovaza.