 New Study On Aspirin and Diabetes: A baby aspirin a day can help prevent a heart attack, according to the experts. If you are in the throes of a heart attack, it is recommended that you take a chewable aspirin. We all know there are numerous cases where the use of over-the-counter aspirin can be helpful to the extent that it can save lives.
New Study On Aspirin and Diabetes: A baby aspirin a day can help prevent a heart attack, according to the experts. If you are in the throes of a heart attack, it is recommended that you take a chewable aspirin. We all know there are numerous cases where the use of over-the-counter aspirin can be helpful to the extent that it can save lives.
A goal of a recent study in Canada was to see whether taking aspirin could prevent a first or second heart attack or stroke in those with diabetes.
That newly released study has given results on the use of aspirin as a preventative measure for heart disease and the recurrence of episodes in patients with diabetes. The study was carried out at the University of Alberta, Canada, by researcher Scot Simpson, an Associate Professor in the Faculty of Pharmacy and Pharmaceutical Sciences.
Simpson concluded that diabetic patients who had already suffered a cardiac or stroke condition who were taking a “low” dose of aspirin daily had “very little benefit” in terms of preventing a second heart attack or a decreased risk of mortality. But, the patients taking “higher” doses of aspirin showed a significantly lower risk.
The researchers took the results from 21 different studies and zeroed in on diabetic patients who had already had a heart attack or stroke to see how aspirin could prevent a second episode. The results were that when taking 325 milligrams of aspirin per day there was a 23 percent lower risk of death.
Simpson stated that people with diabetes have an increased risk of cardiovascular disease, “adding there is evidence that suggest as much as 60 percent of deaths in diabetics is attributable to heart disease.” Simpson stated that “pharmacists could have an active role” in helping patients with their questions regarding aspirin.
Before making any changes in your medication, always check with your doctor first, especially when it comes to any over-the-counter medication. People with type 2 diabetes, in many cases, take several different medications. The addition of aspirin, without their doctor’s consent, might lead to unnecessary problems and hospitalizations.
Aspirin (acetylsalicylic acid) has been around for many, many years and is most commonly used as an analgesic to relieve minor aches and pains, to reduce fever and is an anti-inflammatory medication.
There are side effects from taking aspirin. These include, but are not limited to, stomach upset, bleeding in the stomach (ulcers), and tinnitus (ringing in the ears), especially at higher doses.
As well, aspirin is no longer recommended for use in children when they are suffering from a cold, the flu or chickenpox or other viral sicknesses because of the risk of Reye’s syndrome.
Take care to always check with your physician before adding aspirin to your medicine routine or increasing the dosage, if you are already taking aspirin. The side effects can be serious and life threatening. Your physician will know your medical history and will be able to advise you on whether or not you should add aspirin on a daily basis and whether or not you should increase the dosage.
 Linagliptin (Tradjenta) Possible Approval for Use in Europe for Type 2 Treatment: Linagliptin (sold under the name Tradjenta) has been available in the United States for those with type 2 diabetes since May 2011, when the Food and Drug Administration gave their approval for its use at that time. Tradjenta is an oral
Linagliptin (Tradjenta) Possible Approval for Use in Europe for Type 2 Treatment: Linagliptin (sold under the name Tradjenta) has been available in the United States for those with type 2 diabetes since May 2011, when the Food and Drug Administration gave their approval for its use at that time. Tradjenta is an oral  Apple Peels, Diabetes and Muscle Wasting: You might not want to peel that apple before eating it, let alone put an apple peel down the garbage disposal or in the trash container under the sink.
Apple Peels, Diabetes and Muscle Wasting: You might not want to peel that apple before eating it, let alone put an apple peel down the garbage disposal or in the trash container under the sink. Zebrafish, Zinc and Diabetes: Zinc is an important trace mineral that people need to stay healthy. Only iron is in stronger form in the body than zinc. Zinc’s highest concentrations are found in the prostate gland and sperm of men, the red and white blood cells, the retinas of the eyes, the liver and the
Zebrafish, Zinc and Diabetes: Zinc is an important trace mineral that people need to stay healthy. Only iron is in stronger form in the body than zinc. Zinc’s highest concentrations are found in the prostate gland and sperm of men, the red and white blood cells, the retinas of the eyes, the liver and the  Study Shows Life Expectancy Longer Now For Type 1 Diabetics:
Study Shows Life Expectancy Longer Now For Type 1 Diabetics:  New Study On Clogged Carotid Arteries And Type 1 Diabetes: Atherosclerosis of the carotid arteries is a buildup of plaque in either the right or left carotid artery, located at the sides on the neck going up to the head. These carotid arteries supply oxygenated blood to the head and neck and are vital for survival. When either of these arteries becomes clogged with plaque, this blood flow to the head and neck can be stopped, and a stroke or a mini-stroke occurs, which could impact a person’s life forever. Usually, the buildup of plaque in the carotid arteries occurs over a period of time.
New Study On Clogged Carotid Arteries And Type 1 Diabetes: Atherosclerosis of the carotid arteries is a buildup of plaque in either the right or left carotid artery, located at the sides on the neck going up to the head. These carotid arteries supply oxygenated blood to the head and neck and are vital for survival. When either of these arteries becomes clogged with plaque, this blood flow to the head and neck can be stopped, and a stroke or a mini-stroke occurs, which could impact a person’s life forever. Usually, the buildup of plaque in the carotid arteries occurs over a period of time. New Drug Delivery Mechanism For
New Drug Delivery Mechanism For 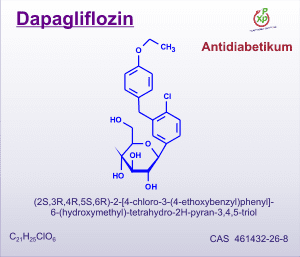 New Drug Potential from Squibb and AstraZeneca for Type 2 Diabetes:
New Drug Potential from Squibb and AstraZeneca for Type 2 Diabetes:  Lee Iacocca has donated over $30 million to diabetes research seeking a cure for the disease, which can lead to debilitating and fatal
Lee Iacocca has donated over $30 million to diabetes research seeking a cure for the disease, which can lead to debilitating and fatal  Hopes for an
Hopes for an