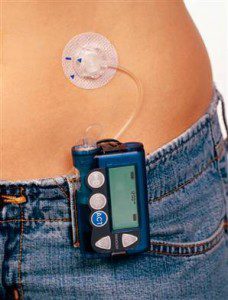
 A recent study has found that insulin pump therapy may be more cost effective than frequent daily insulin injections in Type 2 diabetics who require large doses of insulin throughout the day.
A recent study has found that insulin pump therapy may be more cost effective than frequent daily insulin injections in Type 2 diabetics who require large doses of insulin throughout the day.
According to Phyllis Wolff-McDonagh, DNP, a certified diabetes instructor, pump therapy was less expensive over the long term because the insulin was absorbed more efficiently than with injections. Wolff-McDonagh presented the findings at the annual American Association of Diabetes Educators meeting; the study analyzed results from Type 2 diabetics with heavy insulin requirements, over 150 units per day. In those patients, insulin pumps saved over $12,000 in a four year period.
Type 1 diabetics have long used insulin pumps to supplement their bodies’ insulin deficiencies. Few studies have been conducted on the efficacy of insulin pumps for Type 2 diabetics; however, the existing research shows that they appear to be at least as effective in regulating hemoglobin A1c levels as multiple daily insulin injections; in some cases, insulin pumps have actually been more effective. None of the previous research has considered the cost of injections versus the cost of pumps.
In Wolff-McDonagh’s new study, the researchers studied medical records of 15 adults who ranged in age from 40 to 64. All of the patients had begun using insulin pumps within the seven years prior to the study; all had failed to achieve HbA1c levels under 8% even though they had undertaken multiple insulin injections every day for at least a year.
The results of the study showed that the mean HbA1c level in the participants dropped from 9.4% at the beginning of the study to 8.2% after one year. The participants showed an average increase in body mass index from 38.6kg/m2 at the beginning of the study to 40kg/m2 after one year. Previous research into both Type 1 and Type 2 diabetes have shown similar increases in body weight associated with improved blood glucose regulation; the weight gain is thought to be associated with a reduction in glycosuria, or the excretion of glucose in the urine.
To analyze the cost of using the pumps, the study participants were separated into three groups according to their level of basal insulin use through multiple daily injections; the low-insulin group used less than 100 units per day, the moderate group used 100-150 units per day, and the heavy-insulin group used over 150 units per day. In calculating costs, the researchers took into account the cost of insulin and supplies such as syringes and pumps.
For patients who received four injections per day, the cost was $525 per year, or $2,100 for four years. The cost of pump therapy included $5,250 for the pump plus $1,500 per year for pump supplies, equaling $11,250 over a four year period.
The cost efficiency of pump therapy varied according to the dosage of the patients. For low-dose patients, injections were less expensive than pumps, with the former costing $9,172 for four years versus $14,994 for the latter. For moderate insulin users, the costs were about the same at $22,380 for injections and $23,002 for pump therapy. For heavy insulin users, pumps were much less expensive at $28,826 versus $41,100 for injections. Dr. Wolff-McDonagh added that since insulin pumps afford more efficient glycemic control, they may also ultimately be cheaper for moderate insulin users.
Pump therapy is not popular among Type 2 diabetics because reimbursement is uncommon. To determine eligibility for receiving a pump, Medicare looks at C-peptide levels, which Wolff-McDonagh believes should change: “Medicare needs to re-look at this, but before that can happen, large randomized controlled studies need to be done to see what happens over long periods of time,” she said.